The first wireless implantable temperature sensor has been created by a team of scientists at Northwestern University to identify episodes of inflammation in Crohn's disease patients. The method provides long-term, real-time monitoring and may help physicians take early action to stop or lessen the long-term harm that inflammatory bouts cause.
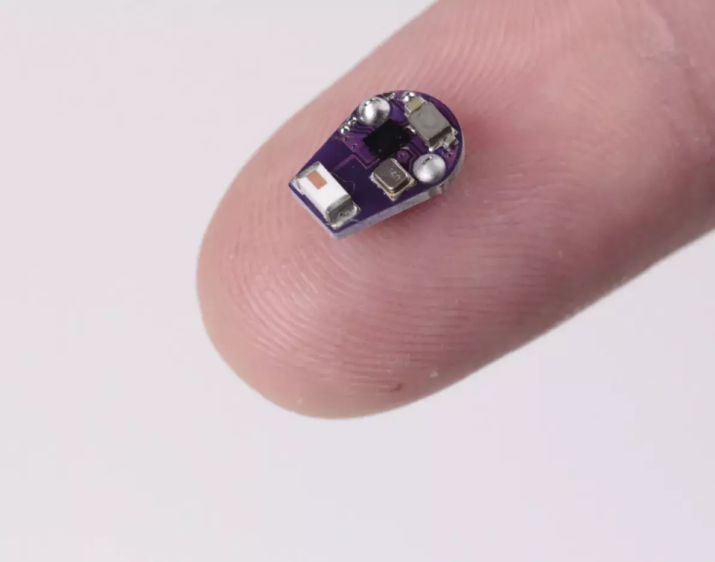 Miniaturized implantable temperature sensor on the finger. Image Credit: Northwestern University.
Miniaturized implantable temperature sensor on the finger. Image Credit: Northwestern University.
Crohn's disease, a chronic inflammatory bowel illness that affects the intestines and can cause digestive problems, weight loss, malnutrition, and other difficulties, affects more than one million people in the United States. Oral treatments are used to treat mild cases, but they usually do not work well over time. As a result, over 70% of Crohn's patients need at least one surgery to remove damaged intestinal segments.
The Northwestern researchers investigated if a temperature sensor gently pressed against the intestines of mice with Crohn's disease may provide real-time information into the disease's course and identify intermittent flare-ups because heat is a sign of inflammation. They succeeded in achieving both objectives in their study, which was published in the journal Nature Biomedical Engineering.
According to Arun Sharma, whose team oversaw the animal research, physicians are presently unable to promptly identify inflammatory episodes, some of which patients are unaware of until the issue worsens to the point where invasive surgery is necessary.
The magnitude of the flareup can be measured with regards to the heat signature, and is it so extensive that it is going to cause tissue damage over time? This could be potentially prevented if a clinician has this information readily at hand and can determine what type of therapy can be given to that person at that moment in time, rather than waiting weeks to get a blood analysis, tissue biopsy, or fecal analysis. In the meantime, you are losing valuable minutes regarding tissue damage with this inflammatory event.
Arun Sharma, Associate Professor and Study Co-Corresponding Author, Department of Urology, Northwestern University
Arun Sharma is also an Associate Professor of Biomedical Engineering at McCormick School of Engineering.
According to Sharma, patients with ulcerative colitis, another inflammatory bowel illness, or any other condition where there is a prolonged inflammatory response may benefit from this method of monitoring temperature swings. The wireless sensors allowed the researchers to continuously monitor temperature changes for over four months during the trial.
In a recent study, bioelectronics pioneer John Rogers and his team, who oversaw the device development, described a soft, ultrathin implant that detects changes in temperature and perfusion to keep an eye on the condition of donated organs.
Once more, the correlation between heat and inflammation was crucial, since increased inflammation surrounding the transplanted organ can serve as a precursor to the patient's immune system rejecting the new organ.
To address Crohn’s disease, we developed an ultraminiaturized, precision temperature sensor with wireless communication capability, and this tiny, soft device takes the form of a smooth, round capsule that rests within the GI system, without affecting natural physiological processes for long-term recordings. The data show some very unique signatures, in the form of perturbations to natural circadian cycles, known as ultradian rhythms, as early indications of inflammatory responses.
John Rogers, Study Co-Corresponding Author, Department of Urology, Northwestern University
According to Surabhi Madhvapathy, a Co-First Author from Rogers group who oversaw sensor engineering, the scientists found that the ultradian temperature rhythms related to cyclic variations in stress levels and inflammatory markers in the blood.
Madhvapathy said, “In addition to the short-term variations, we learned over the span of weeks to months, that the average temperature of the intestines decreases, and this decrease was indicative of the worsening tissue quality over time.”
The researchers intend to evaluate the sensor capabilities in human tissues that replicate the inflammatory gut conditions associated with inflammatory bowel disease after these encouraging results in mice.
Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering and Neurological Surgery at McCormick and Director of the Querrey Simpson Institute for Bioelectronics, which provided funding to the research.
Arun Sharma is Director of Pediatric Urological Regenerative Medicine and Surgical Research at Ann & Robert H. Lurie Children’s Hospital of Chicago and the Stanley Manne Children’s Research Institute, and a member of Northwestern’s Simpson Querrey Institute for Bio Nanotechnology.
The paper's Co-First Authors are Surabhi Madhvapathy from the Rogers group and Matthew Bury from the Sharma group.
Journal Reference:
Madhvapathy, S. R., et al. (2024) Miniaturized implantable temperature sensors for the long-term monitoring of chronic intestinal inflammation. Nature Biomedical Engineering. doi.org/10.1038/s41551-024-01183-w.
Source: https://www.northwestern.edu/