May 9 2013
Innovative projects including: smart-phone test and tracking systems for infectious diseases; fibre optic probes that can monitor people’s condition in intensive care; and in-home sensors that can relay patient information to doctors immediately, have benefitted from a £32 million investment.
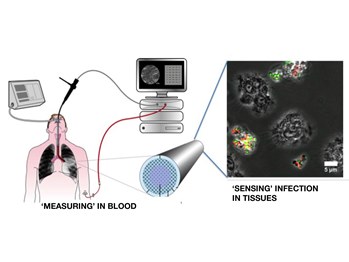 Fibre-optic probe (Edinburgh)
Fibre-optic probe (Edinburgh)
The funding from the Engineering and Physical Sciences Research Council will establish three new Healthcare Interdisciplinary Research Collaborations (IRCs).
Welcoming the centres, David Willetts, Minister for Universities and Science, said: “New British technologies are transforming healthcare and saving lives, for example, in future, our smart phones will tell us when we are ill, controlling the spread of infectious diseases. As healthcare challenges become more complex, our world-class scientists are finding the next generation solutions.”
The technologies being developed by the IRCs are:
- Early-warning sensing systems for infectious diseases - next generation smartphone test and tracking systems for serious infections including new strains of influenza, MRSA and HIV - led by UCL (University College London) with Newcastle University, Imperial College London, and The London School of Hygiene and Tropical Medicine.
- Multiplexed ‘Touch and Tell’ Optical Molecular Sensing and Imaging - a fibre-optic device to detect potentially fatal lung conditions in intensive care patients, and to continuously monitor the blood in critically ill adults and babies without the need for blood sampling. Led by the University of Edinburgh with Heriot-Watt University and the University of Bath.
- SPHERE: Sensor Platform for HEalthcare in a Residential Environment - a 24/7 digital home health assistant. Sensor technology to monitor patient’s health in their own homes targeting obesity, depression, falls, stroke, cardiovascular and musculoskeletal diseases. Led by the University of Bristol with the University of Southampton and University of Reading.
This investment in the three new IRCs will focus UK research excellence and build critical mass in this area, and will be spread across ten universities and involve 18 industry and academic partners. The IRCs will focus on research that can create or use new ICT applications and technologies to determine and/or sense physical and environmental factors, and integrate, analyse and interpret this data to inform decisions.
Dave Delpy, CEO of EPSRC said: “Today’s healthcare challenges are many and complex; designing and integrating technologies that will help clinicians to diagnose and monitor patients is where the cross-disciplinary research we are funding at these IRCs can play a vital role. EPSRC funds projects that can make a real difference to people’s lives, the efficiency of our healthcare system and to the economy.”
Researchers from different disciplines, policy makers, industry and clinicians will work together at the IRCs to ensure that their research leads to the maximum benefit for healthcare users as rapidly as possible.
Notes to Editors:
The total investment into the three IRCs is £41 million: £32 million coming from EPSRC and a further £9 million investment from the Universities and project partners.
Grants have been awarded to three IRCs for these projects:
Early-Warning Sensing Systems for Infectious Diseases, led by Dr Rachel McKendry, UCL, together with Newcastle University, Imperial College London, and The London School of Hygiene and Tropical Medicine. Project partners: Microsoft Research, OJ-Bio Ltd, Mologic Ltd, Cambridge Life Sciences Ltd, Zurich Instruments, O2 Health, UCL Partners: Newcastle Hospitals NHS Foundation Trust. EPSRC Grant awarded - £11 million, total project investment £17 million. Grant ref: EP/K031953/1.
This IRC will develop next generation smart phone technologies that allow doctors to test and track serious infectious diseases – such as new strains of influenza, HIV and MRSA - much earlier than ever before, empowering patients to gain faster access to treatment and protecting the public.
Infectious diseases are one of the greatest threats to human health. Early diagnosis plays a vital role in treatment, care and prevention. However, worldwide, many infections remain undiagnosed and untreated or are diagnosed at the late stage due to poor diagnostic tools. The result is on-going transmission of serious infections and delays in the identification of emerging threats such as pandemic influenza.
This IRC will develop low cost, easy to use smart phone-connected diagnostic tests based on advances in nanotechnology to rapidly diagnose infections in community settings including GP surgeries, elderly care homes, developing countries or even at home. Results will be sent securely to healthcare systems, alerting doctors to potentially serious outbreaks with geographically linked information. The system will also track reported illness and symptoms across populations by searching millions of on-line sources including internet searches and social media posts to identify outbreaks even before people attend clinics or from resource-limited settings.
Worldwide there are an estimated 6.8 billion mobile phone subscriptions and 2.7 billion people on-line, with rapid expansion in developing countries.
Dr Rachel McKendry, Director of this IRC, explains: “A new generation of diagnostic test and tracking systems could save millions of people from deadly diseases such as new strains of influenza, HIV and MRSA. The revolution in mobile communication, nanotechnology, genomics, and ‘big data’ analysis offers tremendous opportunities to ‘actively’ manage outbreaks and ultimately to prevent infectious diseases. I am delighted to bring together some of the very best researchers in the UK to create innovative 21st century technologies in the battle against infectious diseases.”
The IRC will bring together critical mass and multi-disciplinary expertise in biomarker discovery, biomimetic capture coatings, nanosensing systems, nanoparticles, microelectronics, microfluidics, wireless networks, data mining and health economics.
To meet the needs of end users, the team will work closely with leading NHS clinicians from UCL Partners and Newcastle Hospitals NHS Trusts, NIHR Biomedical Research Centres, Public Health England, industry, regulators, patient groups and the public. The centre also benefits from links to more than 100 countries in Africa, Asia and South America.
Multiplexed ‘Touch and Tell’ optical molecular sensing and imaging led by Professor Mark Bradley, University of Edinburgh, together with Heriot-Watt University and the University of Bath. Project partners: ST Microelectronics Limited, Carestream Health, Edinburgh Biosciences Limited, UK Astronomy Technology Centre. EPSRC Grant awarded: £9 million, total project investment £11 million.
Grant ref: EP/K03197X/1.
The IRC will bring together a group of world class scientists and clinicians to design make and test a cutting-edge bedside technology platform - a small fibre optic probe which can be inserted into the patient’s lung, blood vessels or other parts of the body such as the digestive, genitourinary or reproductive tracts.
Initially the research will focus on patients in intensive care units (ICU), and critically ill babies.
The probe will help doctors in the ICU make rapid and accurate diagnoses that would inform therapy and ensure patients get the right treatment, quickly.
Potentially fatal lung complications are a common problem in ventilated ICU patients. Currently, doctors caring for these patients in the ICU face many challenges, often needing to make snap decisions without the information necessary to properly inform their choices. The technology platform developed in this programme will give doctors important information on the conditions of ICU patients and whether they have infections, inflammation or scarring in their lungs.
Using advanced fibre optic technology, micro-electronics and new sensor arrays the ground-breaking solution is to create a novel fibre-based probe that can readily be passed into the gas exchanging areas of the lung and blood vessels of ICU patients.
The probe will house a variety of special optical fibres, some of which allow clinicians to ‘view’ inside the lung while others will be modified with sensors that can measure important parameters such as oxygen concentration and acidity in both blood and lung in real-time. In addition the fibre will deliver 'smart reagents' that detect specific bacteria and viruses and sense other processes that can damage the lung.
When integrated together these signals will provide highly specific information about the degree and type of lung damage and the potential causative 'bug' if an infection is suspected. Because of the large amount of information generated and in order to make it easily interpreted by doctors, computing experts will convert these signals into easy-to-understand disease readouts.
Research will also look at improving healthcare for critically ill babies by using the probe. Critically ill babies often need to have blood samples taken to test for oxygen and acid levels – by inserting a probe into their circulation these levels will be continuously monitored without the need for taking the blood from the baby.
Professor Mark Bradley, Director of the Edinburgh IRC who will be leading the interdisciplinary team, said: “This fantastic team of multi-disciplinary scientists and clinicians will work seamlessly together to produce a solution to radically improve how disease is detected, monitored and treated in critically ill patients.”
SPHERE: Sensor Platform for HEalthcare in a Residential Environment - led by Professor Ian Craddock, University of Bristol, with the University of Southampton and University of Reading. Project Partners: IBM United Kingdom Limited, Toshiba Research Europe Limited, Bristol City Council, NIHR BRU Nutrition, Diet & Lifestyle, Bristol Health Partners, and Knowle West Media Centre(KWMC). EPSRC Grant awarded: £12 million, total project investment: £15 million. Grant ref: EP/K031910/1
Britain’s obese and ageing population is at risk of isolation, depression, strokes and fractures caused by falls in the home. SPHERE will develop a 24/7 digital home sensor system to monitor the health and wellbeing of people with different health challenges living at home.
An example of SPHERE’s home sensor system could be to detect an overnight stroke or mini-stroke on waking, by detecting small changes in behaviour, expression and gait. It could also monitor a patient’s compliance with their prescribed drugs.
Professor Ian Craddock, Director of this IRC, said: “Families, carers, health and social services professionals involved in all stages of care will benefit from the system. SPHERE will address real world challenges by developing a practical technology to target health concerns such as; obesity, depression, stroke, falls, cardiovascular and musculoskeletal diseases.”
The system will be general-purpose, low-cost and accessible. Sensors will be entirely passive, requiring no action by the user and suitable for all patients including the most vulnerable.
Home medical sensor technology is seen by many engineers and academics as the future, however, it will also be seen by many in society as a highly-invasive and undesirable replacement for face-to-face care.
SPHERE’s community and user-centric approach to developing a low-cost useable home sensor platform is proposed as the ideal environment to develop a sensor system that is of value to clinical, industrial and citizen stakeholders.
SPHERE will work hand-in-hand with the local community. It will develop practical, user-friendly technologies and pilot systems in a large number of homes over extended periods of time. Leading clinicians in heart surgery, orthopaedics, stroke and Parkinson’s disease, and recognised authorities on depression and obesity will also be involved.