Jan 11 2021
For people struggling with obesity or suffering from serious health-related problems due to weight gain, gastric bypass surgery, at times, becomes the last option.
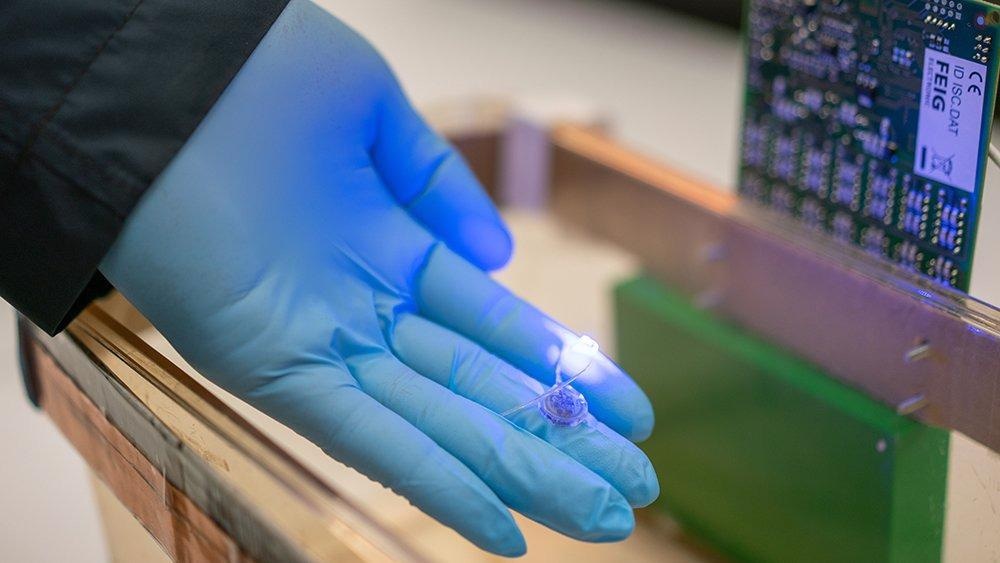 Park’s paddle-shaped device consists of a harvester that contains microchips for wireless communication. The harvester also produces currents to power LEDs inserted near the end of the shaft. Image Credit: Matthew Linguist, Texas A&M Engineering.
Park’s paddle-shaped device consists of a harvester that contains microchips for wireless communication. The harvester also produces currents to power LEDs inserted near the end of the shaft. Image Credit: Matthew Linguist, Texas A&M Engineering.
In gastric bypass surgery, a small stomach pouch is created and the digestive tract is rerouted, which not only makes this procedure highly invasive but also extends the recovery period for the affected patients.
Now, in a recent study, scientists from Texas A&M University have explained a new medical device that may help people to lose weight and needs an easier surgical procedure for implantation.
According to the team, the new centimeter-sized device offers the feeling of fullness by activating the vagus nerve endings with light. The researchers’ device is different from other devices that need a power cord because it is wireless and can be externally controlled from a distant frequency source.
We wanted to create a device that not only requires minimal surgery for implantation but also allows us to stimulate specific nerve endings in the stomach. Our device has the potential to do both of these things in the harsh gastric conditions, which, in the future, can be hugely beneficial to people needing dramatic weight-loss surgeries.
Sung II Park, Assistant Professor, Department of Electrical and Computer Engineering, Texas A&M University
The study results have been published in the January issue of the Nature Communications Journal.
For individuals who have at least two obesity-associated conditions, or have a body mass index of more than 35, surgery provides an option to them to lose their excess weight and also maintain their weight over the long term.
The vagus nerve provides sensory data about the feeling of fullness from the stomach lining to the brain and, as a result, it has lately received a great deal of attention as a target for treating obesity.
While medical devices are there that can activate the ends of the vagus nerve and thus help control hunger, such devices have almost the same design as that of a pacemaker, with wires linked to a current source that sends electrical jolts to stimulate the nerve tips.
According to Park, wireless technology and the application of sophisticated optical and genetic tools have the ability to render nerve stimulation devices more comfortable and less cumbersome for patients.
Despite the clinical benefit of having a wireless system, no device, as of yet, has the capability to do chronic and durable cell-type specific manipulation of neuron activity inside of any other organ other than the brain.
Sung II Park, Assistant Professor, Department of Electrical and Computer Engineering, Texas A&M University
Hence, to bridge this gap, Park and his group initially applied genetic tools to express light-responsive genes into the ends of the specific vagus nerve in vivo. They subsequently developed a very small, paddle-shaped device and embedded micro LEDs close to the tip of its flexible shaft, which, in turn, was attached to the stomach.
In the head of the device, known as the harvester, the researchers accommodated the microchips required for the new device to wirelessly interact with an external radio frequency source. Besides, the harvester was designed to generate small currents to power the micro LEDs. The researchers then switched on the radio frequency source and demonstrated that the light produced by the LEDs was effective at curbing hunger.
The team added that they were rather surprised to find that the biological machinery that synchronizes the suppression of hunger in their experiments was different from traditional wisdom. A widely accepted fact is that the stomach expands when it is full and the data about the stretch is transmitted to the brain through mechanoreceptors found on the vagus nerve.
Our findings suggest that stimulating the non-stretch receptors, the ones that respond to chemicals in the food, could also give the feeling of satiety even when the stomach was not distended.
Sung II Park, Assistant Professor, Department of Electrical and Computer Engineering, Texas A&M University
Looking ahead, Park added that the new device may also be utilized to exploit nerve endings across the gastrointestinal tract and other organs, such as the intestine, with little or no changes.
“Wireless optogenetics and identifying peripheral neural pathways that control appetite and other behaviors are all of great interest to researchers in both the applied and basic fields of study in electronics, material science and neuroscience,” added Park. “Our novel tool now enables interrogation of neuronal function in the peripheral nervous systems in a way that was impossible with existing approaches.”
Others who contributed to the study include Woo Seok Kim, Sungcheol Hong, and Milenka K. Gamero from the electrical and computer engineering department; Vivekanand Jeevakumar, Clay M. Smithhart, and Theodore J. Price from The University of Texas at Dallas; and Richard D. Palmiter and Carlos Campos from the University of Washington.
The study was funded by grants from the interdisciplinary X-Grants Program, a NARSARD Young Investigator Award from the Brain and Behavior Research Foundation, the National Science Foundation’s Engineering Research Center for Precise Advanced Technologies and Health Systems (PATHS-UP), and the University of Washington Diabetes Research Center and the National Institutes of Health.
Journal Reference:
Kim, W. S., et al. (2021) Organ-specific, multimodal, wireless optoelectronics for high-throughput phenotyping of peripheral neural pathways. doi.org/10.1038/s41467-020-20421-8.
Source: https://www.tamu.edu/