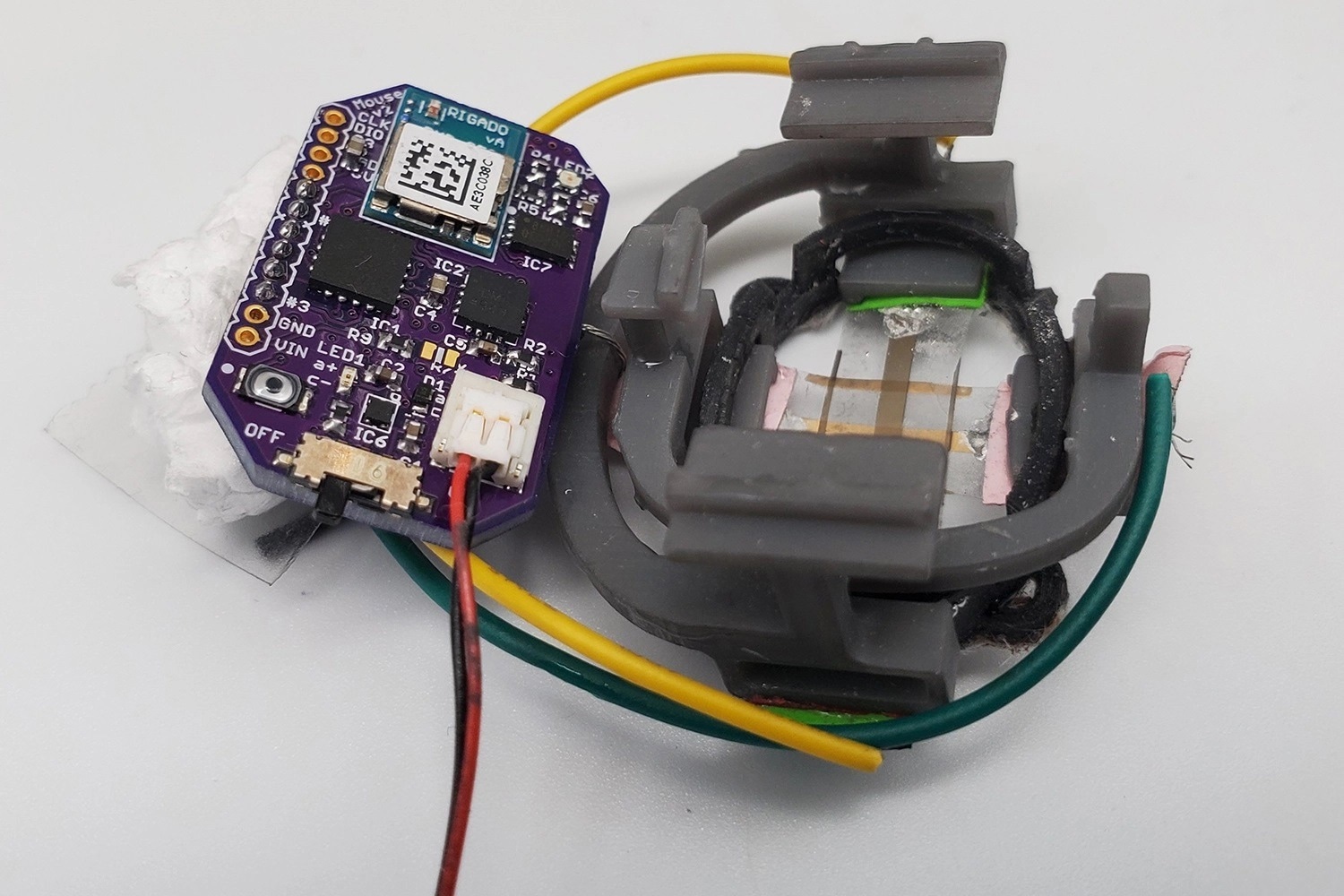
The FAST system measures tumor size regression and is a new way to test the efficacy of cancer drugs. Image Credit: Alex Abramson, Bao Group, Stanford University.
The battery-functioned, non-invasive device is responsive to one-hundredth of a millimeter (10 micrometers) and can wirelessly send results to a smartphone app with just a button press in real-time.
The researchers say that, in practical terms, their device “Flexible Autonomous Sensor measuring Tumors” or “FAST”, signifies an entirely novel, quick, cheap, hands-free, and precise method to assess the efficiency of cancer medications. On a larger scale, it could likely result in new cancer treatment approaches. FAST is described in a paper reported on September 16th, 2022, in Science Advances.
Scientists assess thousands of potential cancer drugs on mice with subcutaneous tumors every year. Some could reach human patients, and the procedure for identifying new treatments is tedious because technologies for quantifying tumor regression from drug therapies take several weeks to receive a response.
Drug screenings are made challenging and labor-intensive through the integral biological changes of tumors, the drawbacks of current measuring methods, and the comparatively small sample sizes.
In some cases, the tumors under observation must be measured by hand with calipers.
Alex Abramson, Study First Author, Stanford University
Abramson is also a recent postdoc in the lab of Zhenan Bao, a K.K. Lee Professor of Chemical Engineering at the Stanford School of Engineering.
Using metal pincer-like calipers to quantify soft tissues is unsuitable, and radiological methods cannot offer the continuous data required for real-time detection. FAST can diagnose alterations in the tumor's volume on the minute scale, whereas caliper and bioluminescence measurements usually need weeks to observe changes in tumor size.
The Power of Gold
FAST's sensor is made of a stretchable and flexible skin-like polymer, which comprises an embedded layer of gold circuitry. Developed by former postdocs and co-authors Yasser Khan and Naoji Matsuhisa, this sensor is attached to a small electronic backpack.
The strain on the membrane — how much it shrinks or stretches — is measured by the device, and that data is transferred to a smartphone. Prospective treatments related to tumor size regression can be confidently and quickly omitted as unsuccessful or fast-tracked for more studies using the FAST backpack.
The scientists state that the new device provides at least three significant advances depending on the research with mice. Firstly, it offers uninterrupted monitoring since the sensor is connected to the mouse physically and stays in place for the entire experimental period.
Secondly, the flexible sensor enshrouds the tumor and can eventually quantify shape changes that are challenging to discern using other approaches. Thirdly, FAST is both non-invasive and independent. Unlike an adhesive bandage, it is connected wirelessly to the skin and battery-operated.
The mouse has complete freedom to move unencumbered by the wires or the device, and researchers need not actively manage the mice following sensor placement. FAST packs can be reused, are just $60 or so to assemble, and can be connected to the mouse in minutes.
The innovation is in the flexible electronic material of FAST. A layer of gold is coated on top of the skin-like polymer, which develops tiny cracks when stretched, changing the material’s electrical conductivity. Stretching the material increases the number of cracks, which increases the sensor’s electronic resistance. As the material contracts, the cracks come back into contact, and conductivity increases.
Characterization of crack propagation and exponential changes in conductivity can be equated mathematically with variations in volume and dimension by Abramson and co-author Matsuhisa, who is an associate professor at the University of Tokyo.
One challenge the scientists had to overcome was the concern that the sensor itself may compromise measurements by putting undue pressure on the tumor, efficiently squeezing it. To avoid that risk, they meticulously equated the flexible material’s mechanical properties to the skin to make the sensor as flexible and supple as real skin.
It is a deceptively simple design. But these inherent advantages should be very interesting to the pharmaceutical and oncological communities. FAST could significantly expedite, automate, and lower the cost of the process of screening cancer therapies.
Alex Abramson, Study First Author, Stanford University