Dementia’s complexity lies not just in its progression, but in its unpredictability. Traditional assessment methods rely heavily on episodic clinical evaluations or caregiver reporting, both of which are prone to underreporting and delay. Most recently, continuous, passive sensing systems have become the tool of choice when it comes to monitor behavioral and physiological changes in real time.
This article explores how wearable and ambient sensors are being used to support people living with dementia, not just by tracking data, but by helping caregivers understand changes in behavior, spot early signs of decline, and provide more responsive, personalized care.
Download your PDF copy now!
What is Dementia? Understanding Causes, Symptoms, Diagnosis and Treatment
The Challenge of Monitoring Dementia
Dementia affects approximately 57 million people globally, with over 10 million new cases of dementia each year worldwide.1 As the condition progresses, patients often experience memory loss, confusion, wandering, sleep disturbances, and difficulty with daily tasks. For families and care providers, monitoring these changes safely, without being invasive, is one of the greatest challenges.
Someone in the world develops dementia every 3 seconds. There are over 55 million people worldwide living with dementia in 2020. This number will almost double every 20 years, reaching 78 million in 2030 and 139 million in 2050. Much of the increase will be in developing countries. Already 60% of people with dementia live in low and middle income countries, but by 2050 this will rise to 71 %.
Alzheimer's Disease International
This is where sensor-based technologies come in: enabling passive, continuous monitoring that can detect early signs of decline, prevent accidents, and improve the quality of care without compromising independence.
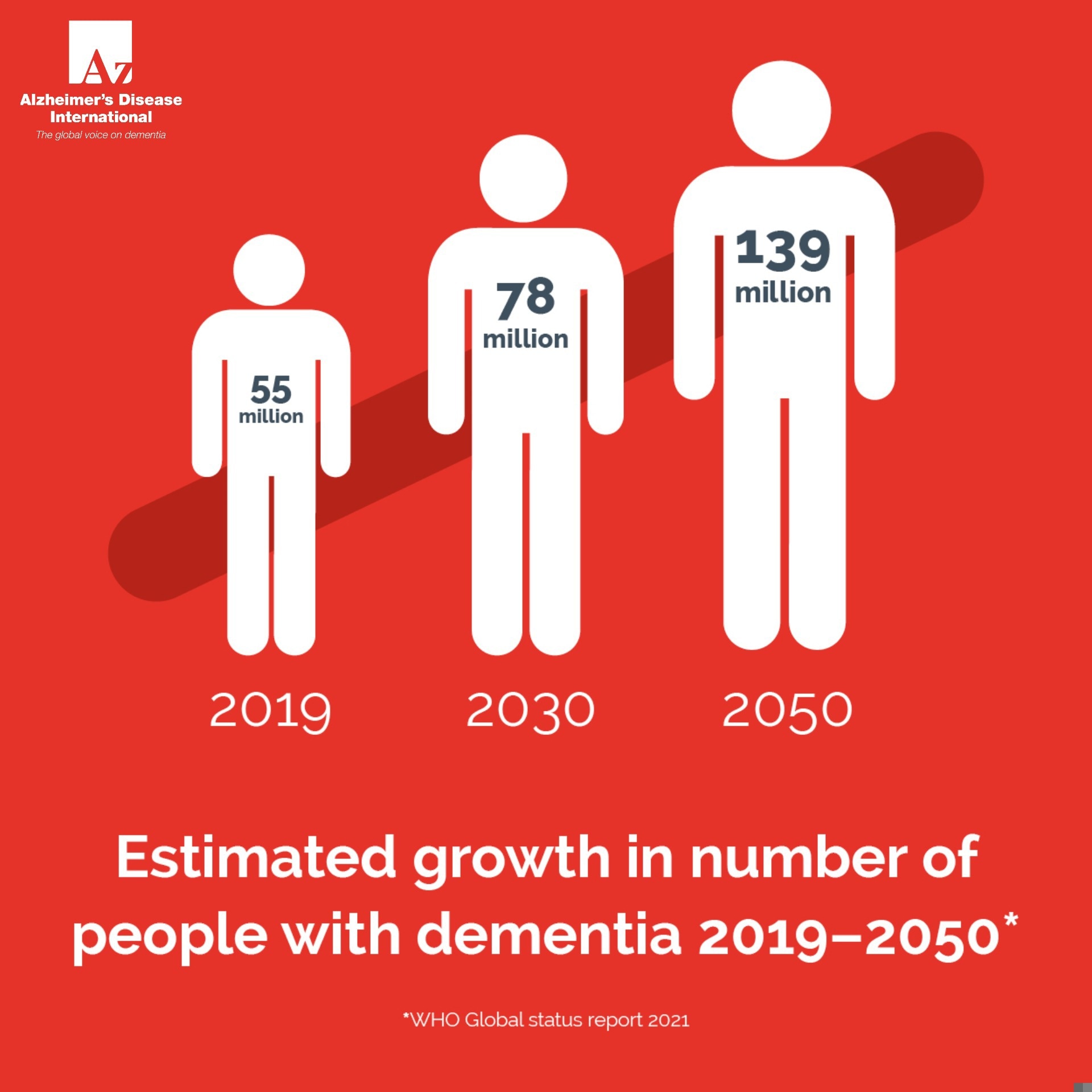
Image Credit: Alzheimer's Disease International
The Sensor Solution: Moving from Episodic to Continuous Care
This shift toward continuous monitoring is about collecting more data as well as recognizing patterns that can inform meaningful interventions. Whether worn on the body or installed throughout the home, today’s sensor technologies are increasingly tailored to the specific needs of dementia care.
Wearable Sensors in Dementia Care
In dementia care, wearables go beyond general wellness tracking. Devices like the Empatica E4 or Withings ScanWatch combine multiple sensing modalities to give clinicians a window into subtle physiological changes that often precede clinical symptoms.
Wearables are already widely used for fitness and chronic disease management, but in dementia care, their value lies in fall detection, heart rate and sleep tracking, as well as GPS tracking.
- Multi-Sensor Detection for Falls and Wandering: Wrist-worn devices with accelerometers, gyroscopes, and GPS can detect atypical motion patterns - such as rapid directional changes or unsteady gait - and issue alerts before a fall or disorientation escalates.
- Skin Conductance and Heart Rate Variability: Some devices measure electrodermal activity, which can correlate with stress, agitation, or confusion, common in mid-to-late-stage dementia but often underreported.
- Passive Monitoring of Sleep-Wake Cycles: Instead of relying on caregiver observations, wearables can automatically track sleep latency, interruptions, and REM patterns. Persistent disturbances may signal discomfort, sundowning, or medication issues.
These aren’t just data streams, they're clinical touchpoints. When connected to care platforms like CarePredict or Kardian, data can be reviewed asynchronously by healthcare providers to tailor treatment plans or adjust care routines.
Ambient and Passive Sensing at Home
Beyond wearables, ambient sensors allow for hands-off, non-stigmatizing monitoring. But their true power comes from the specificity of what they track and how those inputs can be interpreted in context.
- Radar-Based Motion Sensors (e.g., Xandar Kardian): Unlike basic infrared sensors, radar sensors detect micro-movements like breathing patterns or restlessness - useful for identifying nighttime agitation or early respiratory issues.
- Pressure-Sensitive Flooring (e.g. SensFloor): These systems map movement patterns across a room, detecting subtle changes in step length, balance, or hesitation - all of which can signal cognitive or physical decline weeks before clinical symptoms emerge.
- Smart Appliance Monitoring (e.g., Howz): By tracking when and how frequently appliances like kettles or TVs are used, these systems can alert caregivers to deviations in routine, such as skipping meals or remaining sedentary for long periods.
- Bathroom Visit Patterns via Water Flow Sensors: Sudden increases in nighttime bathroom visits can be a red flag for urinary tract infections - a common but often overlooked trigger of confusion or agitation in older adults with dementia.
What sets these tools apart is their passive nature. They don’t require users to wear, charge, or interact with anything directly, making them ideal for individuals who may forget or resist wearable devices.
Integrated into care-home networks or private homes, these devices give loved ones peace of mind while preserving a person’s sense of independence.
As part of our exploration into sensor technologies in dementia care, we spoke with Simon Lord, Head of Innovation at Alzheimer’s Society, about how innovation is being used to meet both the clinical and emotional needs of people living with dementia.
This Dementia Action Week, we’re highlighting the most common symptoms of dementia and encouraging anyone with concerns to use our free symptom checklist and seek help from their GP or other health professional.
More than a third of people with dementia don’t have a diagnosis, meaning they’re missing out on the vital care, support and treatment they need. At Alzheimer’s Society, we support and invest in innovative solutions to address the challenges people affected by dementia face today, while our world-class research helps to deliver the treatments of tomorrow.
Simon Lord, Head of Innovation at Alzheimer’s Society
One example is a newly announced collaboration between two of the Society’s Innovation Partners: HUG™ by LAUGH, a sensory product designed for comfort, and Milbotix, creators of SmartSocks that track wellbeing indicators like stress. “Together, they are developing a Smart HUG to monitor heart rate and stress, providing measurable evidence for non-pharmacological interventions in dementia care,” Lord explained.
He also shared that the Alzheimer’s Society will be exhibiting for the first time at London Tech Week, showcasing emerging technologies that aim to improve the quality of life for people with dementia. “Our Innovation team will be at London Olympia from 9 to 11 June, engaging with industry leaders to explore how we can all contribute to better dementia care."
The Role of AI and Analytics
Collecting data is only part of the story. The real value lies in interpreting it in ways that inform care decisions and, ideally, before a crisis occurs. That’s where machine learning and predictive analytics step in.
Modern platforms like CarePredict and SafelyYou don’t just report that a person got out of bed at 3 am, they learn what’s typical for each individual, then flag what’s not.
- Predictive Fall Risk Models: By analyzing gait patterns from wearable sensors and correlating them with past incidents, AI can anticipate fall risks days or even weeks in advance. SafelyYou, for example, uses computer vision in memory care facilities to capture unwitnessed falls and analyze footage for contributing environmental or behavioral factors.
- Behavioral Trend Detection: Continuous data feeds on mobility, sleep, and hygiene habits can highlight early signs of cognitive decline, infections, or medication side effects. For instance, a sudden drop in kitchen activity combined with increased sleep interruptions might prompt a clinical review.
- Anomaly Detection Over Time: AI models can distinguish between an isolated irregularity and a sustained behavioral change. This makes alerts more meaningful and helps prevent false alarms that often lead to caregiver fatigue.
The goal isn’t to replace human judgment but to enhance it, giving caregivers and clinicians timely, context-rich insights they can act on.
Challenges and Ethical Considerations
Technology in dementia care exists within an ethical landscape that can’t be overlooked. These systems often monitor individuals who may have limited capacity to give informed consent or fully understand the nature of the technologies in use. This reality demands thoughtful design, careful deployment, and ongoing dialogue with all stakeholders involved.
In the early stages of dementia, clear and repeated communication about what data is being collected - and why - is essential. As the disease progresses, the responsibility for consent may shift to families or legal guardians, but the emphasis on transparency shouldn’t diminish. People living with dementia deserve to be treated not just as care recipients, but as individuals with agency, wherever possible.
Privacy is another central concern. Many sensor platforms rely on cloud-based infrastructure, which raises valid questions about who owns the data, how securely it’s stored, and who gets to access it. Limiting data collection to what’s clinically relevant, ensuring encryption and GDPR-compliant practices, and being transparent about data use policies can go a long way in building trust.
Equally important is the need to avoid overloading caregivers with constant alerts. A flood of notifications, especially false or low-priority ones, can quickly lead to alert fatigue, making it harder to spot the truly urgent signals. Effective systems should allow for customizable thresholds, prioritize alerts based on context, and build in smart escalation protocols to ensure interventions are timely and appropriate without becoming overwhelming.
Finally, it’s crucial to remember that technology is a support tool, not a substitute for human care.
No sensor or algorithm can replace the intuition, empathy, and judgment that experienced caregivers bring.
The most effective solutions are those that integrate seamlessly into existing care workflows, provide adequate training, and are co-developed with input from frontline staff who understand the realities of dementia care on a day-to-day basis.
By keeping these ethical considerations front and center, we can ensure that innovation in dementia care remains grounded in respect.
Conclusion: Keeping Innovation Human-Centered
Sensors are reshaping how we approach dementia care, making it more responsive, preventative, and attuned to the day-to-day realities of those affected. By enabling earlier detection of risk, creating safer living environments, and supporting more personalized interventions, these technologies offer meaningful tools in a space that often struggles with limited time and resources.
But for these tools to truly make a difference, they need to be developed and deployed with empathy and collaboration. That means engineers working alongside clinicians and caregivers, involving people living with dementia in the design process, and ensuring that ethical concerns - like consent, privacy, and autonomy - aren’t afterthoughts.
The goal isn’t just smarter care, but better care: grounded in dignity, informed by data, and delivered by people who understand that no technology can replace human connection.
Want to Learn More?
If this article has taken your interest, why not consider looking into some of the below topics?
Download your PDF copy now!
References and Further Reading
- World Health Organization. https://www.who.int/news-room/fact-sheets/detail/dementia#:~:text=Key%20facts,nearly%2010%20million%20new%20cases.
- Alzheimer's Disease International. https://www.alzint.org/about/dementia-facts-figures/dementia-statistics/
- Yang, P., Bi, G., Qi, J. et al. Multimodal Wearable Intelligence for Dementia Care in Healthcare 4.0: a Survey. Inf Syst Front 27, 197–214 (2025). https://link.springer.com/article/10.1007/s10796-021-10163-3
- Chan, L.L.Y. et al. (2025) ‘Daily-life walking speed, running duration and bedtime from wrist-worn sensors predict incident dementia: A watch walk – UK biobank study’, International Psychogeriatrics, p. 100031. https://www.sciencedirect.com/science/article/pii/S1041610224046015